As a trainer and cycle instructor, I have several clients who refuse to do jumping jacks, jump rope, or pedal out of the saddle in class. No, they aren’t lazy or unmotivated. These are confident, competent, fit women who work hard to get and stay in shape. So why do they shy away from certain exercises? Because they, like thousands of women, are scared of bladder leakage putting a damper on their workout—and their spirits.
“Urinary incontinence can affect every aspect of a woman’s life,” says Dr. Alex Runnels, OBGYN and owner of Scarlett Phoenix Cosmetic and Reconstructive Gynecology. “It can take her from being able to fully enjoy all activities to being so limited that it can lead to depression, anxiety, weight gain, and overall decreased satisfaction in all areas of life.”
Why It Happens

Contrary to popular belief, bladder leakage is not limited to women who have experienced childbirth. Although it’s true that childbearing can have what Runnels describes as a “drastic effect on the integrity of the tissue supporting the continence mechanisms,” there are plenty of other factors. Obesity is one. These include conditions such as chronic coughing, anatomic or structural defects, high-impact activities, and the natural aging process. Then there are those women who are simply genetically predisposed to suffer from urinary incontinence.
“The overall incidence in adult women is somewhere between 40-70% depending on the demographic,” says Runnels. “So yes, it is an extremely common problem.”
While it’s nothing to be embarrassed about, bladder leakage is also not something you have to endure. Depending on the severity of the problem, various treatment options are available to help you feel more comfortable and confident.
Physical Therapy and Behavior Modifications
The least invasive (and least expensive) way to treat mild urinary incontinence is through physical therapy and behavior modifications. Making adjustments to your diet by limiting your intake of caffeinated beverages and alcohol can help, along with practicing deep breathing and relaxation techniques when the urge to urinate strikes. Retraining your body to urinate at specific times is another approach, and of course, practicing those Kegels, the pelvic floor exercise designed to help strengthen the muscles surrounding the bladder and urethra. The best way to find those muscles is to stop urinating midstream. Once you’ve identified the muscles, you can practice the technique anytime. In fact, once you’ve mastered the technique, it is best NOT to practice it while urinating, as that can lead to infection by not allowing the bladder to fully empty.
State-Of-The-Art-Technology
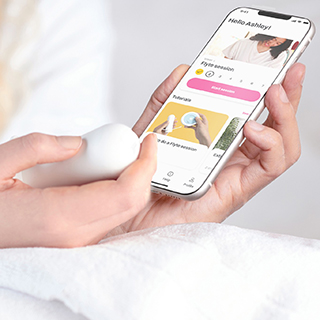
If remembering to do Kegels throughout the day feels like one more thing to check off your to-do list, consider non-invasive Flyte. This physician-recommended device delivers gentle mechanotherapy—therapeutic mechanical stimulation—to the pelvic floor muscles with a discreet vaginal wand. In just five minutes a day, Flyte strengthens the pelvic floor and delivers continence results comparable to those of surgery, without the need for a scalpel.
Botox Injections
Not just for your face, Botox is now being injected into the bladder to help the muscles relax. This treatment is most effective for those who suffer from leakage due to the frequent or sudden urge to urinate, versus those who experience leakage due to “stress” such as coughing or exercise. However, if you struggle with both, which many women do, it can be an effective weapon in your arsenal because it buys you more time to get to the bathroom when the “urge” strikes.
Surgical Slings
As the name suggests, this common surgical procedure for treating stress incontinence involves inserting a mesh hammock-type device underneath the urethra. The sling eliminates leakage by lifting and supporting the urethra (along with the neck of the bladder) with great results. Although it is a relatively quick outpatient procedure, it is more costly than other treatments, and there is some discomfort and downtime post-surgery.
The O-Shot®

No, it’s not something you order at the bar. It’s a quick, effective, relatively pain-free in-office procedure that not only puts an end to leakage, but it can also improve your sex life. Talk about a win/win!
“The O-Shot® offers a solution that falls in between wearing pads, taking medications, and the more extreme treatments like surgeries,” says Runnels, who explains that it was initially designed to repair sexual dysfunction and enhance sexual function, but was found to have been even better at treating urinary incontinence.
The procedure injects the body’s own platelet-rich plasma (PRP) into two different areas of the vagina to promote significant growth and regeneration of lost tissue in the pelvis surrounding and supporting the urethra.
“The result is a thicker, stronger muscle mucosal tissue and glandular tissue associated with maintaining urinary continence,” explains Runnels, adding that it is important that the PRP prep device is FDA approved and that the provider has been licensed by the Cellular Medicine Associates (CMA).
The entire procedure usually takes under an hour and is relatively painless. There is no downtime required, and patients can resume all normal activities, including exercise and intercourse, the same day. While some patients experience an improvement in leakage on the first day, the longer-lasting effects of the procedure occur approximately three weeks later, with the full effect happening around the 9-to-12-week mark. Results typically last from six months to three years, depending on the patient’s aging process, tissue integrity, and lifestyle.
Of course, the only way the O-Shot® or any treatment works is if you speak up about your issues. Many women are embarrassed to discuss bladder leakage with their doctors, a problem Runnels hopes to see disappear in the near future.
“Women need to give themselves permission to take care of themselves,” she says, adding that when women neglect their own health issues it makes it harder for them to take care of everyone else. “The message here is that women deserve to ask questions and feel like they have a right to do things for themselves that improve their quality of life, especially in the arena of vaginal health, and urinary and sexual function.”
Read Next:
Intimacy, Hormones, and Bladder Leaks







